Read and report vaccine reactions, harassment and failures.
What is the history of Meningococcal Disease in America and other countries?
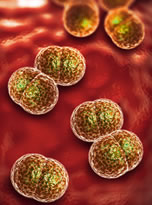
The first reports of invasive meningococcal disease were noted as far back as the 16th century, however, it was Swiss physician Gaspard Vieusseux who, in 1805, definitely described the disease. In 1884, two Italian pathologists became the first researchers to describe the meningococcal bacteria, and in 1887, it was determined to be the cause of bacterial meningitis after being isolated in samples of cerebral spinal fluid collected from six infected individuals. During the First World War, at a time when meningococcal disease rates were noted to be significantly higher, the classification of strains (currently referred to as serogroups) began with the discovery of at least two distinct strains of the bacteria.
Meningococcal infections presenting as meningococcal meningitis became a nationally reportable disease in the U.S. as early as the first part of the 20th century. In the early 1900’s, between 69 and 90 percent of cases were fatal, with fatality rates higher among children than adults. Between 1913 and 1916, the disease was reported at a rate of two cases per 100,000 population.
In 1917-1918, meningococcal meningitis disease rates rose significantly, however, in 1919, rates began decreasing steadily and continued to do so over a five-year period before returning to the low pre- World War I rates. In the U.S., between 1924 and 1927, the disease rate was again reported at two cases per 100,000 population, while in Europe, the rate was noted to be at 1.4 cases per 100,000 population.
Between 1918 and 1928, horse antiserum was primarily used to treat meningococcal meningitis and public health officials reported that the antiserum was relatively successful in decreasing mortality rates from the disease. However, by 1928, when both meningococcal meningitis disease and death rates rose significantly, treating physicians frequently reported the antiserum to be completely ineffective. In 1929, during an epidemic of meningococcal meningitis, approximately 11,000 cases and 5,208 deaths were reported. While public health officials acknowledged that disease rates had increased significantly during this epidemic, they also reported that meningococcal disease was still very rare. They did, however, express concerns about the high number of fatalities associated with the disease.
In the latter part of the 1930s, researchers began experimenting with sulfonamides as a potential treatment for meningococcal disease. Certain experiments involved the use of a sulfonamide, such as sulfanilamide, or sulfapyridine alone or administered along with horse antiserum. Public health officials reported that the use of horse antiserum in combination with a sulfonamide appeared to be most effective.
The last reported epidemic of meningococcal disease occurred in 1943-1944. In 1943, there were 18,223 reported cases of meningococcal disease, however, by 1950, the disease rate had significantly decreased and only 3,788 cases were reported that year.
In 1952, public health officials reported infants to be four times more likely than school children and adults to develop meningococcal disease and that the disease was more likely to spread in overcrowded populations. Further, upon evaluation of the four meningococcal disease epidemics occurring between 1915 and 1951, health officials noted that two took place during war time and two during a time when industrial activities had significantly increased. As a result, they concluded that meningococcal disease outbreaks were more likely to occur during periods of high travel and at times when individuals relocated from a rural setting to more populated urban setting.
In the 1950s and 1960s, meningococcal disease strains resistant to sulfonamides began to emerge, prompting a change in treatment protocols to include the use of antibiotics such as penicillin and chloramphenicol. While penicillin can still be used to treat the disease, medical experts currently consider cephalosporins the antibiotic of choice against invasive meningococcal disease. In 1960, there were 2,259 reported cases of meningococcal disease and the death rate was report to be 0.4 per 100,000 population.
Between 1964 and 1968, meningococcal serogroup B was found to be responsible for the majority of disease cases, however, in 1969, meningococcal serogroup C disease emerged in both military and civilian populations. By 1972, meningococcal serogroup B re-emerged and accounted for the majority of cases. Serogroup C was still found to be responsible for at least one-third of meningococcal cases. When the first meningococcal serogroup A and C polysaccharide vaccines were licensed for use in the United States in 1975, they were ineffective against meningococcal serogroup B, which was the strain responsible for most cases of invasive meningococcal disease. In 1975, there were 1,478 reported meningococcal cases and 308 related deaths.
In 1985, when the CDC’s Advisory Committee on Immunization Practices (ACIP) made its first recommendations on the recently licensed tetravalent meningococcal polysaccharide vaccine targeting serogroups A, C, Y, and W-135 for use in persons with functional or anatomic asplenia or terminal complement component deficiencies, serogroup B accounted for between 50 to 55 percent of all meningococcal disease. Meningococcal serogroup C accounted for 20-25 percent, followed by serogroup W-135 at 15 percent, serogroup Y at 10 percent and serogroup A at 1-2 percent. At this time, there were 2,479 reported cases of meningococcal disease, and the disease rate was reported to be at 1.04 cases per 100,000 population.
There was an average of 2,400 cases of meningococcal disease reported yearly between 1992 and 1996, with disease rates higher among infants and adults 30 years of age and older. Serogroup C accounted for 35 percent of cases, followed by serogroup B at 32 percent, and serogroup Y at 26 percent. Meningococcal polysaccharide vaccines were administered primarily during an outbreak of the disease as the vaccine offered only short-term protection and was ineffective in children under the age of two.
From 1998 to 2007, and prior to the introduction of meningococcal conjugate vaccines targeting serogroups A, C, Y, and W-135, meningococcal disease rates continued to decrease. By 2007, there were 1,077 reported cases of meningococcal disease, down significantly from the 2,725 cases reported in 1998. Disease rates dropped from 0.92 cases per 100,000 population in 1998 to only 0.33 cases per 100,000 population by 2007. Researchers reported that while they could not offer any explanation for the significant decrease in the number of cases of meningococcal disease, they acknowledged that the newly licensed meningococcal conjugate vaccine was not responsible for the reduction in disease rates.
Meningococcal disease from all serogroups declined again from 1,172 reported cases in 2008 to 372 cases in 2015. Serogroup B invasive disease also declined significantly during the same time period even without the availability of a meningococcal serogroup B vaccine. Again, meningococcal disease researchers could not offer any explanation to account for the decrease in the number of reported meningococcal serogroup B disease cases during this time period.
In 2020, there were 235 reported cases and 23 deaths attributed to meningococcal disease. Of the reported cases, serogroup B accounted for 55 cases and 6 deaths; Serogroup C accounted for 54 cases and 2 deaths; Serogroup W accounted for 15 cases and 3 deaths; serogroup Y accounted for 50 cases and 6 deaths; nongroupable serogroups accounted for 26 cases and 3 deaths; and unknown serogroups accounted for 35 cases and 3 deaths.
In January 2022, an outbreak of serogroup C meningococcal disease began, with most cases reported among men who have sex with other men. As of January 2023, there have been 43 cases and nine deaths associated with this outbreak, with thirty-five percent of cases occurring in persons with HIV illness. All cases have occurred in adults between the ages of 20 and 77.
Globally, the World Health Organization (WHO) states that there is an inadequate surveillance system in place to reliably report on the burden of meningococcal disease. This results in a lack of accurate estimates in the number of cases that occur annually. The sub-Saharan desert, an area stretching from Ethiopia in the east to Senegal in the west, has historically accounted for the highest number of meningococcal meningitis cases worldwide. Often referred to as the meningitis belt, WHO reports that approximately 30,000 cases occur annually. Untreated cases of meningococcal disease are reported to have a fatality rate of approximately 50 percent and over 10 percent of individuals who develop the disease suffer severe long-term residual health problems as a result.
NVIC “Quick Facts” is not a substitute for becoming fully informed about Meningococcal disease, meningitis and the Meningococcal vaccine. NVIC recommends consumers read the more complete information following the "Quick Facts", as well as the vaccine manufacturer product information inserts, and speak with one or more trusted health care professionals before making a vaccination decision for yourself or your child.



